
#Joint commission sentinel event verification
Goal 4-to eliminate wrong-site, wrong-patient, and wrong-procedure surgery using a preoperative verification process to confirm documents, and to implement a process to mark the surgical site and involve the patient/family.
Goal 1-to improve the accuracy of patient identification by using two patient identifiers and a “time-out” procedure before invasive procedures. 17 In response to the occurrence of these preventable errors, the Joint Commission issued two National Patient Safety Goals on Januto target wrong-site surgery: 17 Of these, WSSs most commonly occur in orthopedic or podiatric procedures, 5 general surgery, and urological and neurosurgical procedures. From the inception of the Joint Commission’s Sentinel Event program, the number of WSSs reported has increased from 15 cases in 1998, to a total of 592 cases reported by June 30, 2007. The incidence of reported WSS has increased in recent years.

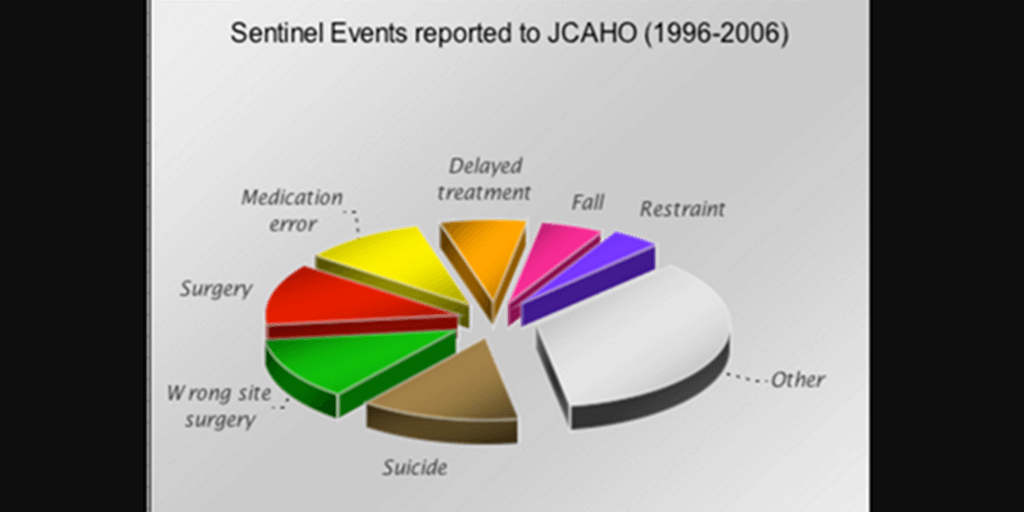
14 Regardless of the exact number of WSSs, they are seen as a preventable medical error if certain steps are taken and standardized procedures are implemented in the perioperative setting. 12 Researchers have confirmed that the Joint Commission’s numbers are low, finding wide variations in the number of WSSs: 1 out of 27,686 cases, 6 or 1 out of every 112,994 surgeries, 13 or 1 in 5 hand surgeons during their career, 7 or 1 out of 4 orthopedic surgeons with 25 years’ experience. Because reporting of sentinel events to the Joint Commission is voluntary, it could be that only 10 percent of actual WSSs are reported. WSSs are rare events, but we are learning more about their prevalence. Indeed, 79 percent of wrong-site eye surgery and 84 percent of wrong-site orthopedic claims resulted in malpractice awards. 9 Surgery performed on the wrong site or wrong person has also often been held compensable under malpractice claims. 6, 7 State licensure boards are imposing penalties on surgeons for WSS, 8 and some insurers have decided to no longer pay providers for WSS or wrong-person surgery, nor for leaving a foreign object in a patient’s body after surgery. WSS can be a devastating experience for the patient and have a negative impact on the surgical team. 5Ĭauses and Consequences of Wrong-Site Surgery WSS is also defined as a sentinel event (i.e., an unexpected occurrence involving death or serious physical or psychological injures, or the risk thereof) by the Joint Commission (formerly called the Joint Commission on Accreditation of Healthcare Organizations), which found WSSs to be the third-highest-ranking event. 3 This definition also includes “any invasive procedure that exposes patients to more than minimal risk, including procedures performed in settings other than the OR, such as a special procedures unit, an endoscopy unit, and an interventional radiology suite” 4 (p. 2 Of great concern is wrong-site surgery (WSS), which encompasses surgery performed on the wrong side or site of the body, wrong surgical procedure performed, and surgery performed on the wrong patient. However, until the 1999 Institute of Medicine report, To Err Is Human, 1 clinicians were unaware of the number of surgery-associated injuries, deaths, and near misses because there was no process for recognizing, reporting, and tracking these events. Surgery is one area of health care in which preventable medical errors and near misses can occur.


 0 kommentar(er)
0 kommentar(er)
